Matakana Island isn’t exactly remote. Guarding the entrance to Tauranga Harbour, you could practically hit a cricket ball across to Mt Maunganui from the southeast corner.
But getting there is another thing. The island is accessible only by boat. There’s no shop, no pub, no doctor if one of the 250 or so inhabitants needs medical treatment, no pharmacy to pick up a prescription.
Yet the mainly M?ori population has high rates of health problems; blood pressure, asthma, allergies, diabetes, heart disease and arthritis are prevalent. In the past, a doctor came to the island once a fortnight, but that wasn’t cost-effective.

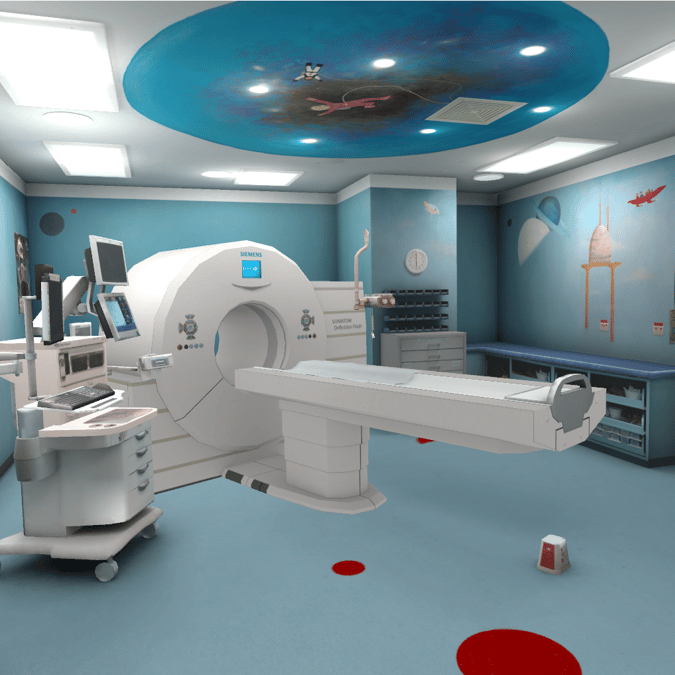
So now a doctor comes every week – by video conference. Patients make an appointment at the community centre and ‘see’ a doctor on the mainland. A nurse is on site to help, and prescriptions are sent to the pharmacy at Omokoroa, and then brought to the island by ferry. If a patient needs to see a doctor in person, they have head into town. But for a regular check-up, it’s an in-out 10-minute job.
Similar telehealth clinics are appearing all around the country, allowing people in remote communities to access a doctor, or sometimes even a specialist, from the nearest medical centre.
But why not from home? These days anyone with a smartphone and a broadband connection can have a Skype conversation, so why would someone needing a routine check-up have to travel to get it, particularly if there’s no hands-on component? That idea is the starting point for New Zealand’s first “virtual health service”, launched in May by the Waikato District Health Board. Patients sign up with their local hospital, download the HealthTap app, and then if their doctor or specialist has registered with the system (and it’s appropriate for their particular treatment) they can choose to have a video conference call or text chat from home or work, rather than travelling to hospital.
“Over 60% of people in the Waikato DHB district live in rural locations and all too often patients are travelling long distances for a short consultation,” says DHB CEO Dr Nigel Murray. “Offering patients the option of a virtual visit will help give everyone access to our services no matter who they are or where they live.”

One of the beauties of the system, says Darrin Hackett, executive director of virtual care and innovation for the DHB, is it’s based on consumer-grade technologies – smartphones, tablets, laptops, plus the sort of clever health apps already being designed by scientists and technicians all around the world: bluetooth weight scales, oxygen and BP monitor apps, fitbits. Not only does this make virtual healthcare more affordable, but it also means in many cases people are using technology they are already familiar with.
The first clinicians to come on board were in dermatology, and already patients are reaping the benefits. Builder Ian Telfer used to have to travel two-and-a-half hours from Whitianga to Hamilton four times a year for a specialist consultation about his itchy skin condition psoriasis. That was basically a whole day away from work for a 15-minute appointment. Now he sees his dermatologist via video conference.
“It’s hard to underestimate the value and importance of a service like this to people who live in remote areas,” Telfer says. “I sat down at home at the end of my working day and switched on the iPad and that’s how we did the consultation. It took no more than 20 minutes.”
Next up will be cardiology and renal specialists, Hackett says. One goal is to move 30% of hospital outpatients visits out to people’s homes or GP surgeries.
The potential benefits for patients who find it hard to get to appointments are obvious. But the service is also designed to meet NZ’s looming demographic healthcare challenge.
“From around 2020, we have a scenario where there’s increasing demand, a significantly decreased workforce and more expensive treatments,” Telfer says. “We recognise we have a short window to make significant change, and part of that is moving services closer to home, and also giving people the tools to make good choices and become more engaged with their own care.”

The message from the Government is the same. Its 2016 Health Strategy involves five key themes for health delivery into the future: people powered; closer to home; value and high performance; one team; and smart system.
The potential is endless. Imagine renal patients on home dialysis with an iPad on the side of their machine so they can access information about their treatment and talk to a clinician if they are having trouble. Or someone who’s been injured talking to a district nurse, showing them the wound on the screen. How about cardiac rehabilitation being done at home by video conference? Or end-of-life care being provided in a patient’s own bedroom, rather than a hospital, but with frequent “visits” from a GP or specialist; all backed up by a 24/7 cover from a team in a regional emergency department?
Mental health (where hands-on treatment is often not needed) is another area where virtual care might make a significant difference, says Dr Jo Scott-Jones, an Opotiki GP and chair of the Rural Health Alliance. At the moment it’s difficult and expensive to provide high quality psychological services in rural areas, he says. However, there’s evidence from overseas that telehealth can make a big difference to outcomes for patients by allowing them to have far more regular contact with a clinician or counsellor.
Another health authority taking an innovative approach is Gore Health, which is trialling a range of mainly broadband-based healthcare technologies to connect rural patients with the care they need. CEO Karl Metzler has big plans for using telemedicine in the future.

“We are looking at setting up a digital follow-up fracture clinic. Let’s say there’s a guy with a broken leg. At the moment, four out of five people with a return fracture appointment have to go to the fracture clinic in Invercargill – that’s a two-hour round trip for what might be a 10-minute appointment. The plan for telehealth is that a specialist in Invercargill would work with a medical officer in Gore to review the fracture over a monitor. No one has to travel; everyone is saved a huge amount of time and money.”
Another area with big potential is opthalmology, he says. There’s a real shortage of ophthalmologists in the southern DHB regions, meaning patients must travel to Dunedin.
“We have a very busy emergency department here – 6000 visits a year, and we have a lot of people with foreign bodies in their eyes. With cameras, eye imaging technology and a digital platform, specialists could assess the problem without the patients having to make the two-hours-each-way trip to Dunedin.”